|
¡¡ |
|
>>Basics
About The Prostate |
|
¡¡ |
|
What
is the prostate? |
Prostate Diseases
|
|
What are prostate
problems? |
Prostate Function |
|
What
is prostatitis? |
Prostate Structure |
|
What tests will my doctor order? |
Female
prostate gland |
|
Why
Does the Prostate Grow? |
Prostate Development |
|
Symptoms Of Prostate Disease |
How
the prostate works? |
|
What
Every Man Should Know |
The Stages of Prostate Growth |
|
What
is prostate enlargement, or BPH? |
What are the side effects of prostate treatments? |
|
|
|
¡¡ |
|
Often
described as a walnut or chestnut-shaped organ,
the prostate is a gland that surrounds the
beginning of the urethra. The prostate produces
a milky fluid that provides nutrient to the
sperm and is discharged into the urethra at the
time of semen emission.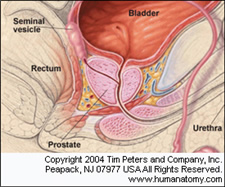
An organ exclusive to men, the development of
the prostate is spurred by male hormones
(especially testosterone). The rate of prostate
growth decreases and may stop around age 20. A
second growth period often occurs around age 45,
as cells in the middle of the prostate start to
reproduce more rapidly than normal. This growth
may result in BPH or enlarged prostate.
The more
you know about the normal development and
function of the prostate, where it¡¯s located,
and what it¡¯s attached to, the better you can
understand how prostate cancer develops and
impacts a man¡¯s life over time¡ªdue either to
cancer growth or as a result of treatments.
Normal Anatomy
The normal prostate is a small, squishy gland
about the size of a walnut (20 milliliters). It
sits under the bladder and in front of the
rectum. The urethra¡ªthe narrow tube that runs
the length of the penis and carries both urine
and semen out of the body¡ªruns directly through
the prostate. The rectum, or lower end of the
bowel, sits just behind the prostate and the
bladder. The normal prostate is composed of
glands and stroma. The glands are seen in cross
section to be rounded to irregularly branching.
These glands represent the terminal tubular
portions of long tubuloalveolar glands that
radiate from the urethra. The glands are lined
by two cell layers: an outer low cuboidal layer
and an inner layer of tall columnar mucin-secreting
epithelium. These cells project inward as
papillary projections. The fibromuscular stroma
between the glands accounts for about half of
the volume of the prostate.
As a male ages, there are more likely to be
small concretions within the glandular lumina,
called corpora amylacea, that represent
laminated concretions of prostatic secretions.
The glands are normally separated by stroma. The
prostate is surrounded by a thin layer of
connective tissue that merges with surrounding
soft tissues, including nerves. There is no
distinct capsule.
Sitting just above the prostate are the seminal
vesicles¡ªtwo little glands that secrete about
60% of the substances that make up semen.
Running alongside and attached to the sides of
the prostate are the nerves that control
erectile function.
Normal Physiology
The prostate is not essential for life, but it¡¯s
important for reproduction. It seems to supply
substances that facilitate fertilization and
sperm transit and survival. Enzymes like PSA are
actually used to loosen up semen to help sperm
reach the egg during intercourse. (Sperm is not
made in the prostate, but rather the testes.)
Other substances made by the seminal vesicles
and prostate¡ªsuch as zinc, citrate, and
fructose¡ªgive sperm energy to make this journey.
Substances like antibodies may protect the
urinary tract and sperm from bacteria and other
pathogens.
The prostate typically grows during adolescence
under the control of the male hormone
testosterone and its byproduct DHT, or
dihydrotestosterone.
Prostate Zones
The prostate is divided into several anatomic
regions, or zones. Most prostate cancer develops
from the peripheral zone near the rectum. That¡¯s
why a digital rectal exam (DRE) is a useful
screening test.
|
Name |
Fraction of gland |
Description |
|
Peripheral zone (PZ) |
Up
to 70% in young men |
The sub-capsular portion of the
posterior aspect of the prostate gland
that surrounds the distal
urethra.
It is from this portion of the gland
that more than 64% of
prostatic cancers
originate. |
|
Central zone (CZ) |
Approximately 25% normally |
This zone surrounds the
ejaculatory ducts.
The central zone accounts for roughly
2.5% of prostate cancers although these
cancers tend to be more aggressive and
more likely to invade the seminal
vesicles. |
|
Transition zone (TZ) |
5%
at puberty |
Prostate cancer originates in this zone
in roughly 34% of patients. The
transition zone surrounds the proximal
urethra and is the region of the
prostate gland that grows throughout
life and is responsible for the disease
of
benign prostatic enlargement.
|
|
Anterior fibro-muscular zone (or stroma) |
Approximately 5% |
This zone is usually devoid of glandular
components, and composed only, as its
name suggests, of
muscle
and
fibrous tissue. |
BPH, a non-cancerous prostate condition,
typically develops from the transition zone that
surrounds the urethra, or urinary tube. This
explains why the condition is typically more
symptomatic than prostate cancer.
Treatment-Related Changes
Because the prostate is close to several vital
structures, prostate cancer and its treatment
strategies can disrupt normal urinary, bowel,
and sexual functioning.
Urinary function¡ªUnder normal
circumstances, the urinary sphincters (bands of
muscle tissue at the base of the bladder and at
the base of the prostate) remain tightly shut,
preventing urine that¡¯s stored in the bladder
from leaking out. During urination, the
sphincters are relaxed and the urine flows from
the bladder through the urethra and out of the
body.
During prostatectomy¡ªthe surgical
removal of the prostate¡ªthe bladder is pulled
downward and connected to the urethra at the
point where the prostate once sat. If the
sphincter at the base of the bladder is damaged
during this process, or if it¡¯s damaged during
radiation therapy, some measure of urinary
incontinence or leakage will occur.
Bowel function¡ªSolid waste that¡¯s
filtered out of the body moves slowly down the
intestines, and, under normal circumstances, the
resultant stool is excreted through the anus
following conscious relaxation of the anal
sphincter. Damage to the rectum caused by
radiation, or more rarely, by surgery, can
result in bowel problems, including rectal
bleeding, diarrhea, or urgency.
Sexual function¡ªIf the erectile
nerves are damaged during prostatectomy, which
was standard during this type of surgery up
until the mid 1980s, the ability to achieve
erection is lost. Sexual desire is not affected,
but severing or otherwise damaging the nerves
can lead to erectile dysfunction. These nerves
can also be damaged by radiation, though this
process usually occurs much more slowly over
time.
Modern techniques in surgery (nerve-sparing),
radiation (intensity modulated radiation
therapy, positioning devices, 3-D conformal
technologies), and seed placement (brachytherapy)
have been developed to try to minimize these
side effects, and this process continues to
improve.
Fertility¡ªAbout 10% of men with
prostate cancer have what is known as seminal
vesicle invasion. This means the cancer has
either spread into the seminal vesicles or has
spread around them. If that occurs, seminal
vesicles are typically removed during
prostatectomy and targeted during radiation
therapy. The loss of the prostate and the
seminal vesicles renders men infertile. After
surgical removal, ejaculation is dry, but
orgasms may still occur. |
|
|
|
Back
To Top |
|
What
is the prostate? |
The prostate is
part of a man¡¯s sex organs. It¡¯s about the size of a walnut
and surrounds the tube called the urethra, located just
below the bladder.
The urethra has two jobs: to carry urine from the bladder
when you urinate and to carry semen during a sexual climax,
or ejaculation. Semen is a combination of sperm plus fluid
that the prostate adds. |
| Article
Source:http://kidney.niddk.nih.gov/kudiseases/pubs/prostate_ez/#What |
|
Back
To Top |
|
What are prostate
problems? |
For men under 50,
the most common prostate problem is prostatitis.
For men over 50, the most common prostate problem is
prostate enlargement. This condition is also called benign
prostatic hyperplasia (BPH). Older men are at risk for
prostate cancer as well, but this disease is much less
common than BPH. More information about prostate cancer is
available from the National Cancer Institute |
| Article
Source:http://kidney.niddk.nih.gov/kudiseases/pubs/prostate_ez/#What |
|
Back
To Top |
|
What
is prostatitis? |
Prostatitis means
the prostate might be inflamed or irritated. If you have
prostatitis, you may have a burning feeling when you
urinate, or you may have to urinate more often. Or you may
have a fever or just feel tired.
Inflammation in any part of the body is usually a sign that
the body is fighting germs or repairing an injury. Some
kinds of prostatitis are caused by bacteria, tiny organisms
that can cause infection or disease. If you have bacterial
prostatitis, your doctor can look through a microscope and
find bacteria in a sample of your urine. Your doctor can
then give you an antibiotic, a medicine that kills bacteria.
Most of the time, doctors don¡¯t find any bacteria in men
with prostatitis. If you have urinary problems, the doctor
will look for other possible causes, such as a kidney stone
or cancer.
If no other causes are found, the doctor may decide you have
a condition called nonbacterial prostatitis.
You may have to work with your doctor to find a treatment
that¡¯s right for you. Changing your diet or taking warm
baths may help. Your doctor may give you a medicine called
an alpha-blocker to relax the muscle tissue in the prostate.
No single solution works for everyone with this condition. |
| Article
Source:http://kidney.niddk.nih.gov/kudiseases/pubs/prostate_ez/#What |
|
Back
To Top |
|
What
is prostate enlargement, or BPH? |
If
you¡¯re a man over 50 and have started having
problems urinating, the reason could be an
enlarged prostate, or BPH. As men get older,
their prostate keeps growing. As it grows,
it squeezes the urethra. Since urine travels
from the bladder through the urethra, the
pressure from the enlarged prostate may
affect bladder control.
If you have BPH, you may have one or more of
these problems:
-
A
frequent and urgent need to urinate. You
may get up several times a night to go
to the bathroom
-
Trouble starting a urine stream. Even
though you feel you have to rush to get
to the bathroom, you find it hard to
start urinating.
-
A
weak stream of urine
-
A
small amount of urine each time you go
-
The feeling that you still have to go,
even when you have just finished
urinating
-
Leaking or dribbling urine
-
Small amounts of blood in your urine
|
|
|
| Article
Source:http://kidney.niddk.nih.gov/kudiseases/pubs/prostate_ez/#What |
|
Back
To Top |
|
How
the prostate works? |
Not all of the
prostate's functions are known. However, one of its main
roles is to provide part of the fluid necessary for
ejaculation. This milky-white fluid in semen provides
nutrients to the sperm so that they can survive long enough
to fertilize an ovum.
The prostate is not part of the urinary system, but because
it surrounds the urethra and sits directly below the
bladder, it can cause urinary problems. That's why your
primary doctor will often refer you to a urologist, a
physician who specializes in the urinary system and male
reproductive system, to see when you are experiencing
prostate problems or prostate disease symptoms. |
| Article
Source:http://www.prostatedisease.org/about_prostate/how_it_works.aspx |
|
Back
To Top |
|
Symptoms Of Prostate Disease |
¡öFrequent
urination
¡öWeak
urine stream
¡öDifficulty
starting urination
¡öBurning
sensation with urination
¡öIncomplete
emptying of the bladder
¡öBlood
or pus in the urine
¡öLoss
of erection
¡öBlood
in semen
¡öBurning
with ejaculation
¡öLow
back pain
¡öDiscolored
semen
¡öInterrupted
urine stream
¡öFrequent
sensation of having a full bladder
¡öOR
NO SYMPTOMS AT ALL |
| Article Source:
http://www.hooah4health.com/prevention/mhealth/symptomsprostate.htm |
|
Back
To Top |
|
What
Every Man Should Know |
Q. Who Gets
Prostate Cancer?
A. Possible risk factors for men: age (including being over
50); having a family history of the disease, and/or being
African American. There is no known cause of prostate
cancer, so a man's best defence against it is annual
prostate exams to aid in early detection of the disease.
Q. What Are Its Symptoms?
A. Symptoms can include frequent urination; difficulty
starting urination; incomplete emptying of bladder; blood or
pus in urine; blood in semen; lower back pain; interrupted
urine stream; weak urine stream, or no symptoms at all.
Q. How Is It Detected?
A. Step One: Prostate cancer is initially detected through
the use of two tests: a digital rectal exam (DRE) and a
prostate specific antigen or PSA blood test. During a DRE, a
doctor inserts a lubricated gloved finger into the rectum
and presses against the prostate gland to check for
abnormalities. The PSA blood test is used to detect elevated
levels of certain protein that may indicate cancer.
Step Two: If the PSA and DRE tests are abnormal, follow up
tests will be done. Transrectal ultrasound provides doctors
with a three dimensional view of the prostate, so they can
determine its size and location prior to biopsy. A needle
biopsy is often performed in conjunction with a transrectal
ultrasound. The surgeon samples small pieces of the prostate
to determine whether BPH, prostatitis or cancer is present.
Q. What Are The Options For Treatment?
A. Prostate cancer is treated according to the state of the
disease. Treatments could include, but are not limited to,
surgery to remove all of the prostate gland, thereby
removing the cancer; radiation therapy, which destroys the
cancer cells; and hormone therapy, which shrinks the size of
the tumor and slows its growth.
Q.
How Successful Is Treatment?
A. Prostate cancer is more easily treated and cured when
detected early. If prostate cancer spreads beyond the
prostate, the outlook is less favorable. Once the cancer has
spread to the lymph nodes and other organs, there is no
cure, only treatment of the disease.
Q. What Are The Possible Side Effects of Treatment?
A. The most serious side effects resulting from prostate
surgery are impotence and incontinence (loss of bladder
control). Impotence may result if the nerves to the penis,
which are very close to the urethra, need to be removed
during surgery. Incontinence may result if the prostate is
removed, because the bladder may lose its ability to hold
back urine.
Q. Can I Protect Myself?
A. Long-term clinical tests to find a method of prevention
are now underway. But for now, two simple tests, a digital
rectal exam (DRE) and a prostate specific antigen (PSA)
performed on schedule can aid in the early detection of
prostate cancer..
Guidelines For Prostate Screening:
All men over the age of 50 should have an annual digital
rectal exam (DRE) and a prostate specific antigen (PSA). Men
with a family history of prostate cancer should check with
their doctors about beginning annual exams at age 40. |
| Article Source:
http://www.hooah4health.com/prevention/mhealth/symptomsprostate.htm |
|
Back
To Top |
|
Prostate Function |
The function of
the prostate is to store and secrete a slightly alkaline (pH
7.29) fluid, milky or white in appearance,that usually
constitutes 25-30% of the volume of the semen along with
spermatozoa and seminal vesicle fluid. The alkalinity of
semen helps neutralize the acidity of the vaginal tract,
prolonging the lifespan of sperm. The alkalinization of
semen is primarily accomplished through secretion from the
seminal vesicles.The prostatic fluid is expelled in the
first ejaculate fractions together with most of the
spermatozoa. In comparison with the few spermatozoa expelled
together with mainly seminal vesicular fluid those expelled
in prostatic fluid have better motility, longer survival and
better protection of the genetic material (DNA).
The prostate also contains some smooth muscles that help
expel semen during ejaculation.
Another important prostate function is controlling the flow
of urine during ejaculation. A complex system of valves in
the prostate, sends the semen into the urethra during
ejaculatory process and a prostate muscle called the
sphincter seals the bladder, thereby preventing urine entry
into the urethra. |
| Article Source:
http://en.wikipedia.org/wiki/Prostate |
|
Back
To Top |
|
Prostate Development |
| The prostatic part
of the urethra develops from the pelvic (middle) part of the
urogenital sinus (endodermal origin). Endodermal outgrowths
arise from the prostatic part of the urethra and grow into
the surrounding mesenchyme. The glandular epithelium of the
prostate differentiates from these endodermal cells, and the
associated mesenchyme differentiates into the dense stroma
and the smooth muscle of the prostate. The prostate glands
represent the modified wall of the proximal portion of the
male urethra and arises by the 9th week of embryonic life in
the development of the reproductive system. Condensation of
mesenchyme, urethra and Wolffian ducts gives rise to the
adult prostate gland, a composite organ made up of several
glandular and non-glandular components tightly fused within
a common capsule. |
| Article Source:
http://en.wikipedia.org/wiki/Prostate |
|
Back
To Top |
|
Female
prostate gland |
The Skene's gland,
also known as the paraurethral gland, found in females, is
homologous to the prostate gland in males. In 2002 the
Skene's gland was officially renamed the prostate by the
Federative International Committee on Anatomical
Terminology.
The female prostate, like the male prostate, secretes PSA
and levels of this antigen rise in the presence of carcinoma
of the gland. The gland also expels fluid, like the male
prostate, during orgasm. Researchers argue that the organ
should therefore be called a female prostate and not "Skene's
gland". |
| Article Source:
http://en.wikipedia.org/wiki/Prostate |
|
Back
To Top |
|
Prostate Structure |
A healthy human
prostate is classically said to be slightly larger than a
walnut. In actuality, it is approximately the size of a kiwi
fruit. It surrounds the urethra just below the urinary
bladder and can be felt during a rectal exam. It is the only
exocrine organ located in the midline in humans and similar
animals.
The ducts are lined with transitional epithelium.
Within the prostate, the urethra coming from the bladder is
called the prostatic urethra and merges with the two
ejaculatory ducts. (The male urethra has two functions: to
carry urine from the bladder during urination and to carry
semen during ejaculation.) The prostate is sheathed in the
muscles of the pelvic floor, which contract during the
ejaculatory process.
The prostate can be divided in two ways: by zone, or by
lobe. |
| Article Source:
http://en.wikipedia.org/wiki/Prostate |
|
Back
To Top |
|
What tests will my doctor order? |
Several tests help
the doctor identify the problem and decide on the best
treatment.
Digital rectal exam. This exam is usually the first test
done. The doctor inserts a gloved finger into the rectum and
feels the prostate, which sits directly in front of the
rectum. This exam gives the doctor a general idea of the
size and condition of the prostate.
Blood test. The doctor may want to test a sample of your
blood to look for prostate-specific antigen (PSA). If your
PSA is high, it may be a sign that you have prostate cancer.
But this test isn¡¯t perfect. Many men with high PSA scores
don¡¯t have prostate cancer.
Imaging. The doctor may want to get a picture of your
prostate using either x rays or a sonogram. An intravenous
pyelogram (IVP) is an x ray of the urinary tract. For an IVP,
dye will be injected into a vein. Later, when the dye passes
out of your blood into your urine, it will show up on the x
ray. A rectal sonogram uses a probe, inserted into the
rectum, to bounce sound waves off the prostate.
Urine flow study. You may be asked to urinate into a special
device that measures how quickly the urine is flowing. A
reduced flow may mean you have BPH.
Cystoscopy. Another way to see a problem from the inside is
with a cystoscope, which is a thin tube with lenses like a
microscope. The tube is inserted into the bladder through
the urethra while the doctor looks through the cystoscope.
|
| Article
Source:http://kidney.niddk.nih.gov/kudiseases/pubs/prostate_ez/#What |
|
Back
To Top |
|
What are the side effects of prostate treatments? |
Surgery for BPH
may have a temporary effect on sexual function. Most men
recover complete sexual function within a year after
surgery. The exact length of time depends on how long you
had symptoms before surgery was done and on the type of
surgery. After TURP, some men find that semen does not go
out of the penis during orgasm. Instead, it goes backwards
into the bladder. In some cases, this condition can be
treated with a drug that helps keep the bladder closed. A
doctor who specializes in fertility problems may be able to
help if backwards ejaculation causes a problem for a couple
trying to get pregnant.
If you have any problems after treatment for a prostate
condition, talk with your doctor or nurse. Erection problems
and loss of bladder control can be treated, and chances are
good that you can be helped.
If your prostate is removed completely to stop cancer,
you¡¯re more likely to have long-lasting sexual and bladder
control problems, such as leaking or dribbling. Your doctor
may be able to use a technique that leaves the nerves around
the prostate in place. This procedure makes it easier for
you to regain bladder control and sexual function. Not all
men can have this technique, but most men can be helped with
other medical treatments. |
| Article
Source:http://kidney.niddk.nih.gov/kudiseases/pubs/prostate_ez/#What |
|
Back
To Top |
|
Prostate Diseases
|
The prostate is a
gland. It helps make semen, the fluid that contains sperm.
The prostate surrounds the tube that carries urine away from
the bladder and out of the body. A young man's prostate is
about the size of a walnut. It slowly grows larger with age.
If it gets too large, it can cause problems. This is very
common after age 50. The older men get, the more likely they
are to have prostate trouble.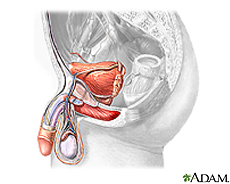
Some common problems are
¡öProstatitis - an infection, usually caused by bacteria
¡öBenign prostatic hyperplasia, or BPH - an enlarged
prostate, which may cause dribbling after urination or a
need to go often, especially at night
¡öProstate cancer - a common cancer that responds best to
treatment when detected early |
| Article Source:
http://www.nlm.nih.gov/medlineplus/prostatediseases.html |
|
Back
To Top |
|
The Stages of Prostate Growth
|
| At birth the
prostate weights around 1.5 grams During puberty the
prostate grows to around 11 grams In the early to middle
20¡¯s the prostate grows to around 18 grams In the early 50¡¯s
there is a new growth phase which continues until around age
70 where the prostate usually reaches around 31 grams. This
phase of growth is what doctors call benign prostatic
hyperplasia (BPH). |
| Article Source:
http://totalprostate.com/prostate_facts.php |
|
Back
To Top |
|
Why
Does the Prostate Grow? |
| There are
conflicting theories as to why the prostate glands growth
goes through these phases. The two theories are based on
changes hormonal levels. |
| Article Source:
http://totalprostate.com/prostate_facts.php |
|
Back
To Top |
| ¡¡ |
|