|
﹛ |
|
Back
To Top |
|
Causes and risk factors of
prostate cancer |
The exact cause of prostate cancer is not known. In
general, cancer is caused by mutations (changes) in the DNA
of cells that cause those cells to grow and divide rapidly.
DNA is inherited from your parents, and about 5% to 10% of
all prostate cancers are due to mutations that were passed
along at conception. If a member of your immediate family
has had prostate cancer, you are at a higher risk of
developing prostate cancer.
Other factors that are considered in a person's risk profile
for prostate cancer include:
Age: the risk of developing prostate cancer increases
significantly after age 50.
Race: prostate cancer occurs 61% more often in
African-American men than in Caucasian men.
Nationality: prostate cancer rates are higher in North
America and northwest Europe and lower in Asia, Africa, and
Central and South America.
Diet: a diet high in fruits and vegetables and low in fat is
considered a good way to reduce the risk of prostate cancer.
Physical activity: keeping physically active and at a
healthy weight may reduce the risk of prostate cancer.
Prostate cancer is
the most common non-skin cancer in America, affecting 1 in 6
men. But who is most at risk of getting prostate cancer and
why?
There are several major factors that influence risk, some of
them unfortunately cannot be changed.
Age: The older you are, the more likely you are to be
diagnosed with prostate cancer. Although only 1 in 10,000
men under age 40 will be diagnosed, the rate shoots up to 1
in 38 for ages 40 to 59, and 1 in 15 for ages 60 to 69.
In fact, more than 65% of all prostate cancers are diagnosed
in men over the age of 65. The average age at diagnosis of
prostate cancer in the United States is 69 years. After that
age, the chance of developing prostate cancer becomes more
common than any other cancer in men or women.
Race: African American men are 60% more likely to
develop prostate cancer compared with Caucasian men and are
nearly 2.5 times as likely to die from the disease.
Conversely, Asian men who live in Asia have the lowest risk.
Family history/genetics: A man with a father or
brother who developed prostate cancer is twice as likely to
develop the disease. This risk is further increased if the
cancer was diagnosed in family members at a younger age
(less than 55 years of age) or if it affected three or more
family members.
In addition, some genes increase mutational rates while
others may predispose a man to infection or viral infections
that can lead to prostate cancer.
Where you live: For men in the U.S., the risk of
developing prostate cancer is 17%. For men who live in rural
China, it*s 2%. However, when Chinese men move to the
western culture, their risk increases substantially.
Men who live in cities north of 40 degrees latitude (north
of Philadelphia, PA, Columbus, OH, and Provo, UT, for
instance) have the highest risk for dying from prostate
cancer of any men in the United States. This effect appears
to be mediated by inadequate sunlight during three months of
the year, which reduces vitamin D levels.
Risk Factors in Aggressive vs. Slow-Growing Cancers
In the past few years, we*ve learned that prostate cancer
really is several diseases with different causes. The more
aggressive and fatal cancers likely have different
underlying causes than slow-growing tumors.
For example, while smoking has not been thought to be a risk
factor for low-risk prostate cancer, it may be a risk factor
for aggressive prostate cancer. Likewise, lack of vegetables
in the diet (especially broccoli-family vegetables) is
linked to a higher risk of aggressive prostate cancer, but
not to low-risk prostate cancer.
Body mass index, a measure of obesity, is not linked to
being diagnosed with prostate cancer overall. In fact, obese
men may have a relatively lower PSA levels than non-obese
men due to dilution of the PSA in a larger blood volume.
However, obese men are more likely to have aggressive
disease.
Other risk factors for aggressive prostate cancer include:
朴
Tall
height
朴
Lack of exercise and a sedentary lifestyle
朴
High calcium intake
朴
African-American race
朴
Family history
Research in the past few years has shown that diet
modification might decrease the chances of developing
prostate cancer, reduce the likelihood of having a prostate
cancer recurrence, or help slow the progression of the
disease. You can learn more about how dietary and lifestyle
changes can affect the risk of prostate cancer development
and progression in PCF*s Nutrition, Exercise and Prostate
Cancer guide.
Risk and Other Prostate Conditions
The most common risk misperception is that the presence of
non-cancerous conditions of the prostate will increase the
risk of prostate cancer.
While these conditions can cause symptoms similar to those
of prostate cancer and should be evaluated by a physician,
there is no evidence to suggest that having either of the
following conditions will increase a man*s risk for
developing prostate cancer.
← Benign Prostatic Hyperplasia (BPH) is a
non-cancerous enlargement of the prostate. Because the
urethra (the tube that carries urine from the bladder out of
the body) runs directly through the prostate, enlargement of
the prostate in BPH squeezes the urethra, making it
difficult and often painful for men to urinate. Learn more
about BPH.
← Prostatitis, an infection in the prostate, is
the most common cause of urinary tract infection in men.
Most treatment strategies are designed to relieve the
symptoms of prostatitis, which include fever, chills,
burning during urination, or difficulty urinating. There
have been links between inflammation of the prostate cancer
and prostate cancer in several studies. This may be a result
of being screened for cancer just by having prostate related
symptoms, and currently this is an area of controversy.
Learn more about prostatitis.
More Myths and Non-Risks
Sexual Activity - High levels of sexual
activity or frequent ejaculation have been rumored to
increase prostate cancer risk. This is untrue. In fact,
studies show that men who reported more frequent
ejaculations had a lower risk of developing prostate cancer.
Having a vasectomy was originally thought to increase a
man*s risk, but this has since been disproven.
Medications - Several recent studies have
shown a link between aspirin intake and a reduced risk of
prostate cancer by 10-15%. This may result from different
screening practices, through a reduction of inflammation, or
other unknown factors.
The class of drugs called the statins - known to lower
cholesterol - has also recently been linked to a reduced
risk of aggressive prostate cancer in some studies.
It*s worth noting that one recent study did show a nearly
twofold risk of developing prostate cancer in men exposed to
Agent Orange.
Alcohol - There is no link between alcohol and
prostate cancer risk.
Vitamin E - Recent studies have not shown a
benefit to the consumption of vitamin E or selenium (in the
formulations studied) in the prevention of prostate cancer.
(Some of the information on this page is adapted from Dr.
Patrick Walsh's Guide to Surviving Prostate Cancer.) |
| Article Source:http://www.prostatedisease.org/prostate_cancer/risk_factors.aspx |
|
Back
To Top |
|
Prostate cancer signs and
symptoms |
Cancer is a serious and life-threatening disease. Yet
many cancers have surprisingly few symptoms. Prostate cancer
is, to a large extent, a silent disease.
In most cases, prostate cancer is detected during a routine
prostate exam. Since many men do not schedule routine rectal
exams, prostate cancer may have already reached an advanced
stage by the time of diagnosis.
When prostate cancer does cause symptoms, they are
frequently confused with those of BPH or enlarged prostate,
a very common condition in men over 55.
Men often associate urinary problems (incomplete urination,
frequent urination, interrupted urine flow, urgency, weak
urine stream, straining to begin urination) with "simply
getting older." But these may be symptoms of prostate
disease, which is why yearly checkups are essential.
Advanced prostate cancer (cancer which has spread to other
parts of the body) often demonstrates more symptoms such as:
Blood in the seminal fluid
Impotence
Back pain and fatigue
However, the lack of these specific symptoms does not mean
that advanced prostate cancer is not present.
When to See a Doctor about Prostate Cancer
See your doctor if you are experiencing any urinary
problems, even if they are not bothersome. Your doctor can
diagnose your condition and, if necessary, advise you about
treatment options.
Not everyone
experiences symptoms of prostate cancer. Many times, signs
of prostate cancer are first detected by a doctor during a
routine check-up.
Some men, however, will experience changes in urinary or
sexual function that might indicate the presence of prostate
cancer. These symptoms include:
←A
need to urinate frequently, especially at night
←Difficulty
starting urination or holding back urine
←Weak
or interrupted flow of urine
←Painful
or burning urination
←Difficulty
in having an erection
←Painful
ejaculation
←Blood
in urine or semen
←Frequent
pain or stiffness in the lower back, hips, or upper thighs
You should consult with your doctor if you experience any of
the symptoms above.
Because these symptoms can also indicate the presence of
other diseases or disorders, such as BPH or prostatitis, men
will undergo a thorough work-up to determine the underlying
cause. |
| Article Source:http://www.prostatedisease.org/prostate_cancer/sign_and_symptoms.aspx |
|
Back
To Top |
|
How prostate cancer is
diagnosed
|
Prostate Cancer Diagnosis
When a doctor finds abnormal results during a Digital Rectal
Examination (DRE) and/or from a Prostate-Specific Antigen (PSA)
test and suspects cancer, the patient will be sent to have a
biopsy.
During a biopsy , samples of prostate tissue are taken
through a small needle that may be inserted into the rectum
or through the perineum into the prostate. An ultrasound
probe inserted into the anus guides the needle. The
procedure is uncomfortable but is usually not very painful.
Prostate Cancer Grading
As part of the diagnosis process, prostate cancer is graded
and staged. The grade describes how aggressive the cancer is
and how fast it is likely to grow.
Most pathologists use the Gleason scale to grade prostate
cancer. They look for the most common type of cancer cell in
the sample and assign it a number between 1 and 5 〞 the
higher the number, the more abnormal the cells are. Another
number is assigned to the second most common type of cell in
the sample. The Gleason score is the sum of these two
numbers (which will be between 2 and 10).
|
T = Tumor |
|
T1: |
Cannot see tumor without using imaging
techniques |
|
T2 - T4: |
Gradiations of sized and/or extent of the
primary cancer |
|
N = Nodes |
|
NO: |
The cancer has not spread to lymph nodes |
|
N1: |
Cancer has spread to the lynph nodes |
|
M = Metastasis |
|
MO: |
No distant metastasis to other organs |
|
M1: |
Metastasis to other organs |
Prostate Cancer Staging
Cancer staging is standardized for most types of solid
tumors. The Staging System of the American Joint
Committee on Cancer (also referred to as the TNM system)
is used most often by doctors to describe a patient's
cancer. The TNM system involves three scores that
describe:
1.The tumor type
2.Whether or not lymph nodes are involved
3.How far the cancer has spread
Once the Gleason Score and the TNM
categories have been established, this information is
combined to determine the cancer*s stage:
Stage I: The prostate cancer cannot be detected
through a DRE or an imaging machine (MRI, CT scan, etc).
Most likely, it was found during a surgical procedure
and has a very low Gleason score.
Stage II: The prostate cancer has not spread to
the lymph nodes or other parts of the body. It was found
during a DRE, PSA, needle biopsy , or transrectal
ultrasound.
Stage III: The prostate cancer has begun to
spread beyond the prostate. It may have spread to the
seminal vesicles, but it has not spread to the lymph
nodes or other parts of the body.
Stage IV: The prostate cancer has spread to tissues next
to the prostate (other than the seminal vesicles), to
lymph nodes, and/or to other, more distant sites in the
body.
|
| Article Source:http://www.prostatedisease.org/prostate_cancer/diagnosis_and_staging.aspx |
|
Back
To Top |
|
Prostate cancer treatment
options |
There are various ways to treat prostate cancer. Before
choosing a treatment, your doctor will consider your age,
health, stage, and grade of disease, as well as your PSA
levels and current medical condition. The common management
options for prostate cancer include:
←Watchful waiting (expectant
management)
←Surgery (radical prostatectomy)
←Radiation therapy
←Hormonal therapy
←Chemotherapy
Since there are several choices available for treating
prostate cancer, doctors often combine methods of treatment,
which is called "combination therapy."
Watchful Waiting
Watchful waiting is based on the premise that the localized
prostate cancer may advance so slowly that it is unlikely to
cause men 每 especially older men 每 any problems during their
lifetimes. Some men who opt for watchful waiting have no
active treatment unless symptoms appear. They are often
asked to schedule regular medical checkups and to report any
new symptoms to the doctor.
In addition to early stage prostate cancer, watchful waiting
is also recommended for small, slow-growing cancer, or for
older men or men with serious medical conditions who may not
handle treatment very well.
Surgery
Surgery is a common treatment for early stage prostate
cancer and may be recommended for patients who are in good
health and younger than age 70.
Radical prostatectomy is usually recommended for early-stage
cancer that has not spread to other tissues or organs. This
procedure makes the patient essentially "cancer free."
During a radical prostatectomy the surgeon removes the
entire prostate gland and sometimes lymph nodes, along with
both seminal vesicles, both ampullae (the enlarged lower
sections of the vas deferens) and other surrounding tissues.
In "nerve-sparing" radical prostatectomy, the nerves to the
penis that control erections are preserved.
Radical prostatectomy typically requires general anesthesia
and takes two to four hours. The patient stays in the
hospital for three days, and needs to wear a tube to drain
urine for 10 days to 3 weeks. Newer techniques for radical
prostatectomy such as laproscopic and robotic prostatectomy
are also available.
Possible side effects of radical prostatectomy
Surgery-related complications, such as bleeding, infection
or cardiovascular problems
Loss or urinary control, called incontinence
Loss of the ability to achieve or maintain an erection
Side effects may be temporary or permanent, depending upon
the patient*s age, extent of disease and type of surgery
Radiation Therapy
Also known as "irradiation" or "radiotherapy", radiation
therapy uses high energy X-rays, either from a machine
(external beam radiation therapy) or emitted by radioactive
seeds implanted in the prostate ("seed implantation" or
brachytherapy, to kill cancer cells. When prostate cancer is
localized, radiation therapy serves as an alternative to
surgery or it may be used after surgery to kill remaining
cancer cells.
External beam radiation therapy generally involves
treatments 5 days a week for 6 to 7 weeks. If the tumor is
large, hormonal therapy may be started at the time of
radiation therapy and continued for several years.
Possible side effects of external beam radiation therapy
Diarrhea
Inflammation of the rectum ("radiation colitis")
Inflammation of the bladder ("radiation cystitis")
Problems with urination
Fatigue
Impotence
With "seed implantation" or brachytherapy, the implantation
procedure is completed in an hour or two under local
anesthesia; the patient typically goes home the same day.
Possible side effects of brachytherapy
Post-implant pain in the rectum
Incontinence
Difficulty in urination (frequency, retention)
Inflammation of the prostate (uncommon)
Sexual impotence (uncommon)
There is no ※one size
fits all§ treatment prostate cancer. You should learn as
much as possible about the many treatment options available
and, in conjunction with your physicians, make a decision
about what*s best for you. Because men diagnosed with
localized prostate cancer today will likely live for many
years, any decision made now will likely reverberate for a
long time.
Your decision-making process will likely include a
combination of clinical and psychological factors,
including:
←The
need for therapy
←Your
level of risk
←Your
personal circumstance
←Your
desire for a certain therapy based on risks, benefits, and
your intuition
Consultation with all three types of prostate cancer
specialists〞a urologist, a radiation oncologist, and a
medical oncologist〞will give you the most comprehensive
assessment of the available treatments and expected
outcomes. Many hospitals and universities have
multidisciplinary prostate cancer clinics that can provide
this three-part consultation service. |
| Article Source:
http://www.pcf.org/site/c.leJRIROrEpH/b.5802089/k.B8D8/Treatment_Options.htm |
|
Back
To Top |
|
Prostate Cancer Prevention |
The ultimate goal
of prostate cancer prevention strategies is to prevent men
from developing the disease. Unfortunately, despite
significant progress in research over the past 16 years,
this goal has not yet been achieved. Both genetic and
environmental risk factors for prostate cancer have been
identified, but the evidence is not yet strong enough to be
helpful to men currently at risk for developing prostate
cancer.
By contrast, some success has been seen with strategies that
can delay the development and progression of prostate
cancer. Studies with finasteride and dutasteride, which are
typically used for men with the noncancerous condition BPH,
have shown that they can reduce by about 25% the chances
that a man will be diagnosed with prostate cancer. The
Prostate Cancer Prevention Trial was one of the largest
prostate cancer trials ever, and involved over 18,000 men
over a decade. This study showed that finasteride was able
to reduce the risk of being diagnosed by 25%, but initially
found a slightly higher rate of aggressive prostate cancers
in men who took finasteride. Later looks at this data have
suggested that this may be an artifact or due to a greater
ability to find more aggressive cancers due to a smaller
gland size (ie a biopsy needle can more easily hit a cancer
in a smaller gland than a larger gland). Given that this
agent is well tolerated, current recommendations call for a
discussion about the risks and benefits of these agents in
the prevention of prostate cancer, and of the potential
risks and benefits of using these agents for other
conditions, such as BPH.
In the meantime, diet and lifestyle modifications have been
shown to reduce the risk of prostate cancer development and
progression, and can help men with prostate cancer live
longer and better lives.
More information about how dietary and lifestyle changes can
be incorporated into everyday life can be found in the
Nutrition, Exercise and Prostate Cancer guide.
Top 10 Considerations for Preventing Prostate Cancer
To understand how to prevent prostate cancer, one must first
understand what causes it. There are four major factors that
influence one's risk for developing prostate cancer, factors
which unfortunately cannot be changed.
Age: The average age at diagnosis of prostate cancer in the
United States is 69 years and after that age the chance of
developing prostate cancer becomes more common than any
other cancer in men or women.
Race: African Americans have a 40% greater chance of
developing prostate cancer and twice the risk of dying from
it. Conversely, Asian men who live in Asia have the lowest
risk; however when they migrate to the west, their risk
increases.
Family history: A man with a father or brother who developed
prostate cancer has a twofold-increased risk for developing
it. This risk is further increased if the cancer was
diagnosed at a younger age (less than 55 years of age) or
affected three or more family members.
Where you live: The risk of developing prostate cancer for
men who live in rural China is 2% and for men in the United
States 17%. When Chinese men move to the western culture,
their risk increases substantially; men who live north of 40
degrees latitude (north of Philadelphia, Columbus, Ohio, and
Provo, Utah) have the highest risk for dying from prostate
cancer of any men in the United States 每 this effect appears
to be mediated by inadequate sunlight during three months of
the year which reduces vitamin D levels.
Given the facts above, which are difficult to change, there
are many things that men can do, however, to reduce or delay
their risk of developing prostate cancer. Why is prostate
cancer so common in the Western culture and much less so in
Asia, and why when Asian men migrate to western countries
the risk of prostate cancer increases over time? We believe
the major risk factor is diet 每 foods that produce oxidative
damage to DNA. What can you do about it to prevent or delay
the onset of the disease?
1.Eat fewer calories or exercise more so that you
maintain a healthy weight.
2.Try to keep the amount of fat you get from red meat
and dairy products to a minimum.
3.Watch your calcium intake. Do not take supplemental
doses far above the recommended daily allowance. Some
calcium is OK, but avoid taking more than 1,500 mg of
calcium a day.
4.Eat more fish 每 evidence from several studies
suggest that fish can help protect against prostate cancer
because they have "good fat" particularly omega-3 fatty
acids. Avoid trans fatty acids (found to margarine).
5.Try to incorporate cooked tomatoes that are cooked
with olive oil, which has also been shown to be beneficial,
and cruciferous vegetables (like broccoli and cauliflower)
into many of your weekly meals. Soy and green tea are also
potential dietary components that may be helpful.
6.Avoid smoking for many reasons. Alcohol in
moderation, if at all.
7.Seek medical treatment for stress, high blood
pressure, high cholesterol, and depression. Treating these
conditions may save your life and will improve your
survivorship with prostate cancer
8.What about supplements? Avoid over-supplementation
with megavitamins. Too many vitamins, especially folate, may
※fuel the cancer§, and while a multivitamin is not likely to
be harmful, if you follow a healthy diet with lots of
fruits, vegetables, whole grains, fish, and healthy oils you
likely do not even need a multivitamin.
9.Relax and enjoy life. Reducing stress in the
workplace and home will improve your survivorship and lead
to a longer, happier life.
10.Finally, eating all the broccoli in the world,
though it may make a difference in the long run, does not
take away your risk of having prostate cancer right now. If
you are age 50 or over, if you are age 40 or over and
African-American or have a family history of prostate
cancer, you need more than a good diet can guarantee. You
should consider a yearly rectal examination and PSA test.
|
| Article Source:
http://www.pcf.org/site/c.leJRIROrEpH/b.5802029/k.31EA/Prevention.htm |
|
Back
To Top |
|
Side
Effects Of Prostate Treatments |
Many men understand that when prostate cancer is caught
early, it can be treated effectively, and the primary
treatment options for localized disease are all excellent
choices. However, many men also have significant concerns
about the side effects of these treatments.
The concerns are justified, but there are many
misunderstandings about how often side effects occur, how
severe they really are and what can be done to manage them
and counteract their occurrence.
Many of the side effects that men fear most following local
treatment are often less frequent and severe than they might
think, thanks to:
Technical advances in both surgery and radiation therapy
Researchers persistently seeking new ways to help overcome
side effects
Improvements in treatment delivery
It*s still important to understand how and why these effects
occur, and to learn how you can minimize their impact on
your daily life.
Categories
There are six broad categories of side effects typically
associated with prostate cancer treatments:
←Urinary dysfunction
←Bowel dysfunction
←Erectile dysfunction
←Loss of fertility
←Side effects of hormone therapy
←Side effects of chemotherapy
Depending on the treatment strategy used, some or all of
these effects might be present. It*s also important to
realize that not all symptoms are normal, and that some
require immediate care.
The below table is an attempt to compare three of these side
effects across the different local therapies (NNSRP=non-nerve
sparing RP, NSRP=nerve sparing RP, EBRT=external beam
radiation therapy, BT=brachytherapy).
Each table shows the proportion of men three years after
therapy with sexual dysfunction (left), bowel problems
(middle), and urinary incontinence (right).
←Yellow indicates normal function
←Blue indicates mild dysfunction
←Red indicates more severe dysfunction
These figures are shown for men with normal function prior
to therapy.
Reproduced from the Journal of Clinical Oncology 2009; 27:
3916-3922.
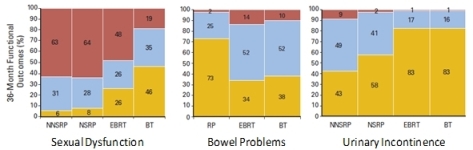
Of
course, exact figures will differ across institutions and
surgeons or radiation oncologists. The figures here are only
meant to be a guide to help understand these risks over
time. The numbers will also differ if there is already
dysfunction present prior to surgery or radiation, as the
risks of side effects are increased in this setting.
While erectile dysfunction rarely improves with any local
therapies compared with before therapy, urinary obstruction
symptoms can often improve after surgery and occasionally
after radiation. Urinary incontinence can also improve after
these local therapies. |
| Article Source:
http://www.pcf.org/site/c.leJRIROrEpH/b.5822789/k.9652/Side_Effects.htm |
|
Back
To Top |
|
Prostate
Cancer Recurrence |
When prostate
cancer is caught in its earliest stages, initial therapy can
lead to high chances for cure, with most men living
cancer-free for five years. But prostate cancer can be slow
to grow following initial therapy, and it has been estimated
that about 20-30% of men will relapse after the five-year
mark and begin to show signs of disease recurrence.
A rising PSA is typically the first sign seen, coming well
before any clinical signs or symptoms. How high is too high
for the PSA to rise to be of concern? At what point should
additional treatment be considered? Which treatments should
be attempted?
In this section, we*ll look at what happens when PSA first
starts to rise after surgery or radiation therapy, and why a
secondary local treatment might be right for you.
The Role of PSA
PSA as a Marker for
Disease Progression
When it comes to assessing disease progression, PSA is
widely accepted as an invaluable tool.
PSA is produced by all prostate cells, not just prostate
cancer cells. At this point in your journey, your cancer
cells have either been removed or effectively killed after
being bombarded with radiation. But some cells might have
been able to spread outside the treatment areas before they
could be removed or killed. These cells at some point begin
to multiply and produce enough PSA that it can again become
detectable by our lab tests.
Therefore, PSA is not really a marker for disease
progression, but a marker for prostate cell activity.
Because the two correlate well after initial treatment for
local therapy, tracking the rise of PSA in this setting is
an important way of understanding how your prostate cancer
is progressing.
However in order to determine whether your PSA is rising,
you need to first determine where it is rising from. Often,
imaging tests will not be able to determine this when the
PSA is at very low levels, however. Tests such as bone
scans, Prostascint scans, and CT/MRI scans in this setting
are often negative and thus most decisions on the next
therapy (ie radiation or hormonal therapy) are based on
probabilities of cure with radiation rather than by seeing
the cancer on scans. Prostascint scans in this setting are
often not very helpful, given their high false positive and
false negative rates, and thus can be misleading.
After prostatectomy, the PSA drops to "undetectable levels,"
typically given as < 0.05 or < 0.1, depending on the lab.
This is effectively 0, but by definition we can never be
certain that there isn*t something there that we*re just not
picking up. By contrast, because normal healthy prostate
tissue isn*t always killed by radiation therapy, the PSA
level doesn*t drop to 0 with this treatment. Rather, a
different low point is seen in each case, and that low
point, or nadir, becomes the benchmark by which to measure a
rise in PSA.
Because the starting point is different whether you had
surgery or radiation therapy, there are two different
definitions for disease recurrence as measured by PSA
following initial therapy.
In the post-prostatectomy setting, the most widely accepted
definition of a recurrence is a PSA > 0.2 ng/mL that is seen
to be rising on at least two separate occasions at least two
weeks apart and measured by the same lab. In the
post-radiation therapy setting, the most widely accepted
definition is a PSA that is seen to be rising from nadir in
at least three consecutive tests conducted at least two
weeks apart and measured by the same lab. It*s important to
always use the same lab for all of your PSA tests because
PSA values can fluctuate somewhat from lab to lab.
The reason that we need to look for confirmation from
multiple tests following radiation is that the PSA can
"bounce" or jump up for a short period after radiation
therapy, and will then come back down to its normal level.
If we relied only on the one elevated PSA, it*s possible
that we will have tested during a bounce phase, and the
results will therefore be misleading. This PSA bounce
typically occurs between 12 months and 2 years following the
end of initial therapy.
If your PSA is rising but doesn*t quite reach these
definitions, your doctor might be tempted to start
initiating further therapy anyway. Remember that PSA is only
one of many factors that help to determine your prognosis
after treatment. The original clinical stage of disease,
your pre-diagnostic PSA, and your overall health and life
expectancy are also key factors in assessing the
aggressiveness of your disease, so be prepared to discuss
treatment options even if you don*t fit the classical
categories for PSA rise after initial therapy.
On the other hand, if your PSA is rising and you do fit the
categories defined above, that doesn*t necessarily mean that
your situation is dire. What researchers have been finding
over the past few years is that universal PSA cut-offs might
not be sufficient for truly understanding how prostate
cancer grows.
PSA Velocity
Suppose one man underwent intensity-modulated radiation
therapy (IMRT), and his PSA nadir was 0.15 ng/mL. Over the
course of nine months, it slowly creeps up until it hits
0.45. But his brother, who also underwent IMRT, nadired at
0.32 ng/mL. If after the same progression over the course of
nine months his PSA also rose to 0.45, are they now in the
same place? Or is there some significance to the fact that
one man*s PSA rose much more rapidly than his brother*s?
The rate at which your PSA rises after prostatectomy or
radiation therapy can be a very significant factor in
determining how aggressive your cancer is, and can therefore
be useful in determining how aggressively it might need to
be treated.
When looking at PSA velocity in a few hundred men who had
undergone either prostatectomy or radiation therapy,
researchers found that men whose PSA doubled in under three
months had the most aggressive tumors and were more likely
to die from their disease, whereas those whose PSA doubled
in more than ten months had the least aggressive tumors and
were less likely to die from their disease.
If we go back to our two hypothetical cases, although both
have a PSA of 0.45 ng/mL, the first one, whose PSA rise
represents a doubling within nine months after treatment,
would likely be considered for an aggressive therapeutic
regimen. And the second case with the smaller rise in PSA?
He might be watched closely to see how rapidly his PSA
rises, and to determine when it might be time to intervene.
However, PSA doubling time or velocity does not always
remain the same over time. So even if you have a very slowly
rising PSA now, continued monitoring with your doctor is
important. Also, if you*ve consistently kept to a very low
PSA rate after treatment, any rise will likely be seen as a
signal that the tumor might be starting to grow again.
Measuring and using PSA velocity is an art, not a science.
There*s no magic number of times that your PSA has to be
tested in order to determine the rate of rise, although most
researchers would agree that more frequent tests over longer
periods of time will likely give a better sense of how your
tumor is growing.
Ultimately, PSA is only one of many factors that can
influence the decision to pursue additional treatments. You
and your doctors will need to weigh all of the different
factors before deciding on the course that*s right for you.
Radiation
Therapy Following Prostatectomy
If your PSA starts to rise after
you*ve undergone prostatectomy,
so-called "salvage" radiation
therapy might be a good option
to explore. With this approach,
external beam radiation is
delivered to the area
immediately surrounding where
the prostate was, in the hopes
of eradicating any remaining
prostate cells that have been
left behind. Radiation is more
commonly being given after
surgery for men with high risk
disease (positive margins,
seminal vesicle invasion,
positive capsular extension),
even in the absence of a PSA
rise. If you did not get
radiation immediately, doing so
later based on a rising PSA is
often reasonable. (Brachytherapy
is not an option because there
is no prostate tissue in which
to embed the radioactive seeds.)
But the procedure is not for
everyone. If there are obvious
sites of disease outside of the
immediate local area, if any
tumor cells have been found in
your lymph nodes, or if your
Gleason score was 8-10,
post-surgery radiation therapy
may not be right for you. In
this high risk situation,
additional therapy may be
warranted such as hormonal
therapies or clinical trials.
Also, in men who are considered
good candidates for this
therapy, it can be very
effective, but five-year
disease-free rates tend to be
considerably higher in men whose
pre-therapy PSA levels are lower
than 0.2 ng/mL compared with
those whose pre-therapy PSA
levels are greater than 0.2 ng/mL.
Therefore, if you and your
doctors are considering
post-surgery radiation, ideally
you should start before your PSA
goes above 0.2-0.4 ng/mL. Side
effects from the radiation
therapy can be moderately
severe, and are additive to
those previously received with
surgery. These include rectal
bleeding, incontinence (urinary
leakage), strictures and
difficulty urinating, diarrhea,
and fatigue. Be sure to discuss
with your doctors what you can
reasonably expect before
deciding on a course of therapy.
In some cases, hormone therapy
might be added for a short
period before radiation to allow
your urinary function to heal,
or during the radiation
treatment, which can also add to
the side effects that you might
experience.
Because the anatomy looks
different and the tumor is often
not visible on imaging or felt
on DRE, the radiation oncologist
has to carefully balance between
delivering sufficient radiation
to destroy the prostate cells
while not damaging the healthy
tissue. Once again, practitioner
skill can make an important
difference in outcomes.
In some cases, particularly if
the tumor was considered
highgrade and therefore at
greater risk of spreading to the
surrounding areas, your doctor
might decide to initiate
radiation therapy right after
you*ve healed from your surgery.
This approach, known as
adjuvant therapy, typically
starts about six weeks after
surgery, and is unrelated to
"salvage" radiation therapy that
is administered if the PSA
begins to rise.
|
| Article Source:
http://www.pcf.org/site/c.leJRIROrEpH/b.5822791/k.1DC2/Recurrence.htm |
|
Back
To Top |
|
Actor
loses long-time battle with prostate cancer |
(NBC) - Dennis
Hopper's acting career spanned more than half a century.
Two of his earliest roles were small parts in major films
starring James Dean--1955's "Rebel Without a Cause", and a
year later, "Giant", which also starred Rock Hudson and
Elizabeth Taylor.
However, it was a counterculture classic in 1969 that made
Hopper a star--"Easy Rider". He not only starred in and
directed the story of freewheeling bikers traveling
cross-country, he also shared an Oscar nomination for the
screenplay with co-star Peter Fonda.
1979 brought Hopper another milestone role--a
photojournalist in Frances Ford Coppola's "Apocalypse Now".
Soon after that role, years of drug and alcohol addiction
caught up with Hopper, nearly costing him his career and his
life.
He talked about getting sober and staying that way in this
1987 interview on today.
"The only thing I worry about: will I have time to live to
do the work I didn't do," said Hopper.
Ironically, it was the role of an alcoholic father and coach
in the 1986 film "Hoosiers" that brought Hopper his second
Oscar nomination as Best Supporting Actor.
In the years since, Hopper made a mark playing memorable
villains, including psychopath Frank Booth in "Blue Velvet"
and vengeful bomber Howard Payne in "Speed".
One of Hopper's most recent roles showcased a lighter touch,
playing a presidential candidate in the 2008 comedy, "Swing
Vote".
A long time art collector, Hopper leaves behind an acting
canvas that was shaded by his hard living lifestyle, but
highlighted by his work on screen.
The actor died Saturday at the age of 74. |
| Article Source:
http://www.wmbfnews.com/Global/story.asp?S=12569133 |
|
Back
To Top |
|
Study
links obesity to more agressive prostate cancer |
WASHINGTON 〞 The
size of a cancerous prostate tumor is directly proportional
to the weight of the patient and the bigger the tumor the
more aggressive the cancer, a study published Wednesday has
found.
"As the patients' body mass index increased, the tumor
volume increased synchronously," said Dr. Nilesh Patil, who
led the six-year study at Henry Ford Hospital in Detroit,
Michigan.
"Based on our results, we believe having a larger percentage
of tumor volume may be contributing to the aggressive nature
of the disease in men with a higher BMI," he said.
The body mass index, or BMI, is calculated by dividing a
person's weight by the square of his or her height.
The doctors established the relationship after analyzing the
cases of 3,327 patients who had cancerous prostate tumors
surgical removed through a robotic procedure.
The subjects of the research were divided into six
categories according to their BMI, with a rating of 24.9
considered normal or underweight, 25 to 29.9 overweight, 30
to 34.9 obese and 40 or higher extremely obese.
The patients' median age was 60 in all the categories.
The researchers weighed each tumor and compared them to a
categorized database of prostate weight.
In each BMI category without exception, they found the
patient's weight was in direct correlation with the size of
the tumor. |
| Article
Source:http://www.google.com/hostednews/afp/article/ALeqM5gH16AGyjQoVsjAmxoBeoNp_cZWcA |
|
Back
To Top |
|
Concern
over prostate cancer treatment |
A leading
cancer specialist in Northern Ireland has said some people
who have prostate cancer would be better off not being
diagnosed.
Dr Anna Gavin, of the NI
Cancer Registry, said
for some older patients
with lower-risk cancers
the effects of treatment
can be more severe than
the disease itself. A
report by the registry
published on Wednesday
found the number of
patients being treated
for prostate cancer in
NI doubled between 1996
and 2006.
It found that one of the
reasons for this was the
increased use of
diagnostic tests such as
PSA.
However, Dr Gavin, one
of the report's authors,
said there was concern
about "over-diagnosis"
of prostate cancer in
the population.
"Many people who are
diagnosed with prostate
cancer live to a very
old age and die of other
things," she said.
"There is quite a debate
now about prostate
cancer and whether
people should have it
detected, because when
it is detected you're on
a path where you have to
be treated and some of
the treatments are
actually quite severe in
terms of their
consequences."
Dr Joe O'Sullivan,
consultant and senior
lecturer in clinical
oncology at the NI
cancer centre, said
doctors were careful not
to give unnecessary
treatment.
"Over-diagnosis is only
really a problem if
there is
over-treatment," he
said.
"There's no doubt that
some prostrate cancers,
it might be better if
they were never
diagnosed in that men
who are diagnosed with
some of the low-risk
cancers it may never
affect them in their
life.
"But once you've been
diagnosed with it, the
key element is not to
treat somebody who
doesn't need treatment."
Protocols
Dr O'Sullivan said
protocols were in place
to try and ensure this.
"There's a really strong
programme put together
called active
surveillance which
addresses this issue,"
he said.
Prostate cancer is the
most common form of the
disease in men in the
UK, accounting for
nearly a quarter (24%)
of all new male cancer
diagnoses.
Its risk is strongly
related to age - very
few cases are registered
in men under 50 and
about three-quarters of
cases occur in men over
65 years. The largest
number of cases is
diagnosed in those aged
70-74.
While more men die with
prostate cancer than
directly from it, Dr
O'Sullivan said it
should still be
regarding as a very
serious disease.
"It is a serious
condition and many
families will have been
bereaved by prostrate
cancer," he said.
"It does often require
quite tough treatment."
Tests
Liz Atkinson, of the
Ulster Cancer
Foundation, said men
should go to their GP
and get all the
information they can
before getting a PSA
test for prostate
cancer.
"It is a test that picks
up some prostate cancers
that don't need
treatment and it can set
them off on this path of
treatment that they may
not necessarily always
need.
"Some people going for
the test really do need
to get all the
information about it so
that they can make an
informed choice about
whether they want to
proceed, knowing what
it's going to lead to."
Side-effects from
treatment can include
incontinence problems
and impotence.
Mrs Atkinson said the
active surveillance
programme had been a
good addition to cancer
services.
"They don't always jump
in immediately,
especially for older
men," she said.
"They really do try not
to treat if it's not
going to be needed.
"That's where this
active surveillance
comes in, where it's
really like a close
monitoring so that
they're not treating
before they really need
to." She urged anyone
with concerns about
prostate cancer to call
the UCF helpline on 0800
783339.
|
| Article Source:
http://news.bbc.co.uk/2/hi/northern_ireland/10216598.stm |
|
Back
To Top |
|
Does
drinking coffee cut down the threat of developing advanced
prostate cancer? |
Drinking coffee
may actually turn out to be beneficial to several males.
This is because a new study claims a powerful relationship
between coffee consumption and the reduced danger of
developing deadly and advanced prostate cancers.
The study authors are of the opinion that caffeine is
essentially not the chief factor in this link. The experts
are uncertain as to which constituents of the beverage are
the most vital; as coffee apparently comprise of several
biologically active compounds such as antioxidants and
minerals.
Kathryn M. Wilson, Ph.D., a postdoctoral fellow at the
Channing Laboratory, Harvard Medical School and the Harvard
School of Public Health, commented, ※Coffee has effects on
insulin and glucose metabolism as well as sex hormone
levels, all of which play a role in prostate cancer. It was
plausible that there may be an association between coffee
and prostate cancer.§
In an upcoming examination, Wilson and colleagues apparently
discovered that men who consumed coffee the most appeared to
have a 60 percent reduced risk of advanced prostate cancer
as compared to men who did not drink any coffee. This is
claimed to be the first study of its kind to observe the
overall danger of developing prostate cancer as well as
danger of localized, advanced and fatal disease.
Wilson mentioned, ※Few studies have looked prospectively at
this association, and none have looked at coffee and
specific prostate cancer outcomes. We specifically looked at
different types of prostate cancer, such as advanced vs.
localized cancers or high-grade vs. low-grade cancers.§
By means of the Health Professionals* Follow-Up Study, the
study authors apparently recorded the usual and
decaffeinated coffee consumption of almost 50,000 men every
four years from 1986 to 2006. It was observed that about
4,975 of these men contracted prostate cancer during that
time. They also investigated the cross-sectional link
between coffee drinking and intensities of flowing hormones
in blood samples apparently gathered from a division of men
in the cohort.
Wilson remarked, ※Very few lifestyle factors have been
consistently associated with prostate cancer risk,
especially with risk of aggressive disease, so it would be
very exciting if this association is confirmed in other
studies. Our results do suggest there is no reason to stop
drinking coffee out of any concern about prostate cancer.§
This connection might also aid in comprehending the biology
of prostate cancer and likely chemo prevention measures.
This data was presented at the American Association for
Cancer Research Frontiers in Cancer Prevention Research
Conference. |
| Article
Source:http://www.healthjockey.com/2009/12/08/does-drinking-coffee-cut-down-the-threat-of-developing-advanced-prostate-cancer/ |
|
Back
To Top |
|
Men
'underestimating' prostate cancer |
Men are
underestimating the impact of prostate cancer, research from
Everyman indicates.
According to a survey by the charity, 17 percent of men
believed the disease kills just 1,000 people in the UK each
year, while 23 per cent underestimated the number by half.
Just 15 per cent correctly stated that prostate cancer takes
the lives of 10,000 British men annually - a figure that
translates to more than one man every hour.
Everyman released the research as part of Male Cancer
Awareness Month, which began yesterday on 1 June.
Dermot O'Leary, Patron of the charity, commented that many
men "remain ignorant" about the symptoms and signs of the
disease.
"The Everyman campaign aims to get across this message to
help reduce the incidence of male cancers, which overall
affect 37,000 men in the UK each year," he added.
According to the organisation, it must generate £2 million
each year to fund its centre in Surrey, Europe's first and
only dedicated male cancer research centre. |
| Article Source:
http://www.cafonline.org/Default.aspx?page=19230 |
|
Back
To Top |
|
Red Wine Compound found to halt Prostate Cancer |
A new study has
said that a compound that is found in red wine may help to
prevent cancer of the prostate, a gland in the male
reproductive system.
The compound that is found in red wine is called &resveratrol*.
According to scientists this compound has anti-oxidant and
anti-cancer properties. Interestingly, resveratrol is also
found in grapes, raspberries, peanuts and blueberries.
Now, in this new study, researchers led by Coral
Lamartiniere of the University of Alabama at Birmingham fed
mice the compound and found an 87 percent reduction in their
risk of developing prostate tumors.
It was found that the mice that were given the compound
mixed with their food over seven months showed the highest
cancer-protection effect.
Doctors recommend moderate consumption of alcohol,
particularly wine for both men and women as it provides a
host of benefits with regrds to dementia, increased stamina,
prevention of damage from strokes, and possibly even as a
means to extend one*s life span.
Moderate consumption refers to an average of two drinks a
day for men and one drink a day for women. |
| Article
Source:http://www.healthjockey.com/2007/09/03/red-wine-compound-found-to-halt-prostate-cancer/ |
|
Back
To Top |
| ﹛ |
|
|